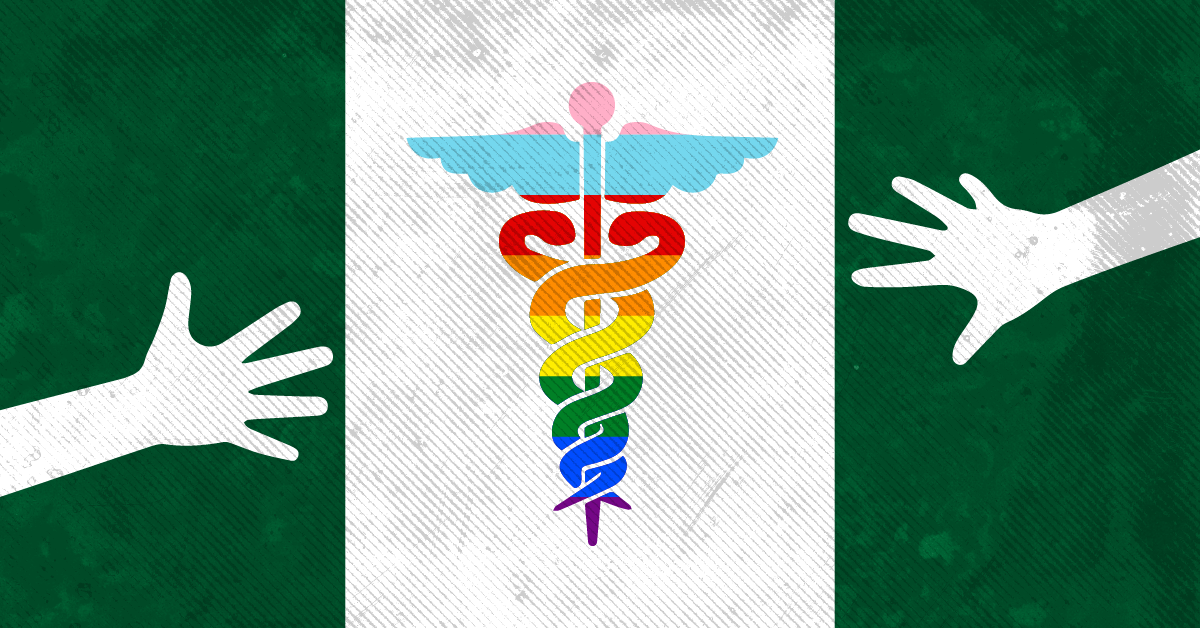
“Over straight allies”: Sexual Minorities in Nigeria turn to peer-to peer education to access medical care
- From individual networks to more organized clinics, here is how sexual and gender minorities in Nigeria receive healthcare.
Lagos, Nigeria (Minority Africa) – In 2017, Kolade*, a bisexual man living in Lagos, experienced discrimination in Nigeria’s healthcare system when he needed a doctor’s consultation for what he perceived to be an anal tear. At first, Kolade sought help from a friend, who was a medical student, but the friend started to ask invasive questions about Kolade’s sexuality.
“I was not comfortable answering his questions because he was straight, so I lied and told him I had very bad constipation instead,” Kolade explains.
Through a WhatsApp group, he was able to find a seemingly open-minded doctor who worked in a state government hospital to whom he spoke freely about his situation.
However, the doctor quickly told Kolade that his condition was not normal and insisted he paid more money for the consultation.
“The doctor charged me 10000 naira (around $14.71) for the consultation when the normal fee for [a] consultation then was 2000 naira (around $2.94) or less, I didn’t mind, I was even willing to pay,” Kolade says.
For his condition, the doctor prescribed Daflon. He however insisted on purchasing the drugs even after Kolade suggested buying the drugs himself. Kolade gave the doctor 15000 naira ($22.06) for Daflon, which in actuality cost 6000 naira ($8.82) in most pharmacies.
When there were no changes to his situation, the doctor suggested a minor surgery to a dismayed Kolade, and after he refused the idea of surgery, the doctor dropped a shocker on Kolade.
“[He] said I should stop having anal sex and I should re-evaluate my lifestyle. I said fuck it and deleted his number,” Kolade says. “It was a friend of mine who revealed to me the doctor was a scam, and he even helped me get the drugs.”
Access to quality health care is supposed to be a fundamental human right, as cited in sections 17(1) & (3) of the 1999 constitution of the federal republic of Nigeria as amended and the National Human Rights Commission (NHRC). This means everyone should be entitled to quality health care services, which include having access to sexual health services free from discrimination and violence.
According to Kolade, this hasn’t been the case in Nigeria, especially for LGBTQ+ people who barely visit public health centers to avoid the discrimination that comes with subpar service or in some cases extortion.
“Minorities will rather self-medicate or reach out to their medical friends than visit a public clinic to treat their sexual health,” he says.
Three years prior, the Same-Sex Marriage (Prohibition) Act of 2013, SSMPA, was passed into law by former president Goodluck Jonathan. Because of this, Kolade couldn’t risk visiting a health center because he feared being jailed, making him vulnerable to extortionists.
Providing equitable access to health care for every Nigerian citizen is central in the country’s National Health Act but the SSMPA has limited the care to only heterosexuals, further driving many LGBT+ members away from public or private hospitals in the country.
However, the tide is changing thanks to non-government organizations like the Community Population Health Initiative (CPHI), which provides primary health care to sexual minorities.
The Community Population for Health Initiative started operations in Nigeria under the international NGO Population Council and they aimed to conduct HIV research to fight against HIV among sexual minorities. In 2020, CPHI transitioned to become an independent clinic that offers sexual health and mental health consultations to sexual minorities at no cost. The clinic prides itself as a safe space for LGBT+ members to voice out their health situations without fear of the consequences attached to their sexuality in the current Nigerian climate. CPHI’s duty is to treat, educate and counsel people who identify as sexual minorities.
Philip*, a 26-year-old software engineer living in Lagos, enjoys watching good TV shows in his free time. It was binge-watching the TV series Pose that led him to get tested for HIV for the first time.
“I visited a public health center to get tested for HIV and all they did was draw my blood and [give] me my result, which was negative by the way,” says Philip.
At that time he was relieved with the result. But when he felt the need for a second test, he chose to visit CPHI after a friend introduced the clinic to him. He admitted to having a better testing experience at CPHI compared to his first experience.
“[At CPHI], I got a small lecture about the virus [and] they also shared safety measures and immediately registered me for PrEP,” Phillip says. “That day I felt like I got a well-rounded HIV testing experience and that satisfied and aided me in making future decisions surrounding my sexual health.”
Even in the face of criminalization, CPHI has chosen to stay defiant and managed to find ways to stay safe while making themselves accessible to sexual minorities. With a license from the government, CPHI can safely care for sexual minorities without being prosecuted by the authorities.
“CPHI operates with a registered license under the corporate affairs commission, the Federal Ministry of Health, and the Lagos state ministry of Health,” says Elizabeth Eshoyemi, the executive director of CPHI.
“But locating sexual minorities in the city and getting them to visit the clinic for testing was difficult, as most of them are too afraid to trust the safety of the clinic.”
In 2015, They began what they call “community outreach” to locate sexual minorities in the area. They were known as population council by this time. They visited private queer hot spots to create awareness and carry out community testing on anyone in need of testing.
In 2017, the Nigeria Police Force (NPF) invaded a private gathering at Ikorodu, Lagos and arrested 40 men on account of engaging in same-sex activities; the NPF arrested 57 men on the same account at Egbeda, Lagos and charged them to court. After those arrests, CPHI had to temporarily stop the outreach for the safety of their staff mostly since the first incident landed one of them in jail.
After they stopped the outreach, they came up with safer ways to reach out to sexual minorities in the city. They train sexual minorities to become peer educators, who are then sent out to the field to educate members of their community. Then they also introduced the Interpersonal Communication method (IPC) also known as peer-to-peer education.
“[Through] IPC, we give queer men and women coupons to encourage them to bring their friends to the facility. For example, someone like me that is easily accessible can invite people to come for tests, even in my home,” Richard Felix, a project coordinator for CPHI, commented.
The IPC approach has proven to be effective over the years, mostly because they use queer men and women to initiate conversations with sexual minorities, as they find it easy to trust members of the community over straight allies.
Often, Felix carries out rapid blood tests for HIV/AIDS which involves using a pin to prick the finger for blood to test for Antibodies/Antigens in the body. The test usually takes between 20-30 mins to get a result.
“Some days I can carry out about eight to ten tests in my home, and we have about over 30 persons engaging the community, which has increased our reach to other states in Nigeria over the years,” Felix says.
Both clients who don’t get the chance to visit the facility or still feel uncomfortable with visiting the facility also get the opportunity to get tested in the privacy of their homes.
“But at the end of the day, everyone still needs facility testing since the home test can sometimes be inconclusive. Facility testing is the best way to get an accurate result,” he adds.
During the Covid-19 lockdown, CPHI initiated a home delivery service. Sexual minorities were able to get their medications delivered to their preferred location. “The home delivery service has also helped us to reach clients that reside outside the city, ” says Esther Uche, a Community Mobilization Officer at CPHI.
Although they work very hard to help create a healthy community, there is no denying that the clinic still faces shortcomings in providing quality health care. The clinic is equipped only for minor, superficial issues, while situations requiring surgeries and other advanced treatments are referred mostly to public hospitals.
“Our government is barely funding anything relating to HIV across the country. All funds come from UNAIDS and Global Fund. It is so sad because [the] government allocates funds for the treatment of this virus, but it has never been used for its intended cause,” Felix laments.
A study has shown that over 81% of funding for HIV comes from international donors, and the government allocates most of the funds to the care of mothers and children living with HIV.
Beyond lack of funding, some clients have also complained about the attitude and the lack of sensitivity of some of the staff in CPHI.
Robyn, a 24-year-old transgender woman, didn’t have a satisfying experience during one of her visits to the clinic. She started visiting CPHI to start the process of her transition and during one of her visits, while waiting at the reception with her friend, a staff member commented a slur about Robyn’s femininity. The employment policy at face value is not necessarily a problem as heterosexual staff claim to be allies, but these experiences underscore the reality that cishet allies can often be insensitive to the experiences of transgender people. As a policy, every staff member must undergo sexual orientation and gender identity expression training (SOGIET).
“When we get complaints through our channels, we investigate and take measures ranging from warnings to suspension and dismissal,” says Eshoyemi.
“I continued to visit the clinic because my friend still worked [there]. After he left, I asked to be transferred to a different NGO that offered almost similar services,” Robyn remarks.
Nonetheless, the quality of care towards sexual minorities has continued to improve, and although still slow-paced, the progress made can’t be ignored. Due to the services from NGOs like CPHI, The Initiative for Equal Rights (TIERS), Heartland Alliance International (HAI), and others existing in the country, sexual minorities still have a chance to live healthy lives.
“We run as a one-stop shop, we provide as many services as we can for sexual minorities to live healthily and earn a living. Sexual minorities are welcome to provide their ideas to help us improve our services,” Eshoyemi tells Minority Africa.
His experience with the healthcare system drove Kolade to become a registered nurse in Nigeria. Today, he works on the frontlines, which grants him access to medical facilities but also he is able to help other sexual minorities get the much needed medical care.
“I really do hope the government can decriminalize all sexuality because I feel that is what keeps most hospitals from actually saving lives in this country” Kolade concludes.
*Names have been changed to protect identities.
Edited or Reviewed by Cassandra Roxburgh, Caleb Okereke, PK Cross, and Uzoma Ihejirika.
Jeffrey Ehijie, A creative writer living in the city of Lagos. His short story “My Testimony” was shortlisted for “Marked” an anthology of short stories about Queer people living with Hiv/Aids. Earlier works has appeared on Tales and Twist anthology and Love Matters. He believes in the power storytelling has to change the human condition.






