I tried teletherapy in Uganda, but is it an “accessible alternative” for everyone?
- Teletherapy gained popularity during the COVID-19 lockdown, enabling people to access therapy from the safety of their homes. With 87% of Uganda’s population living in rural areas and 28 inpatient psychiatric units throughout the country, this alternative may work for some people, while others prefer more traditional or interactive forms of therapy.

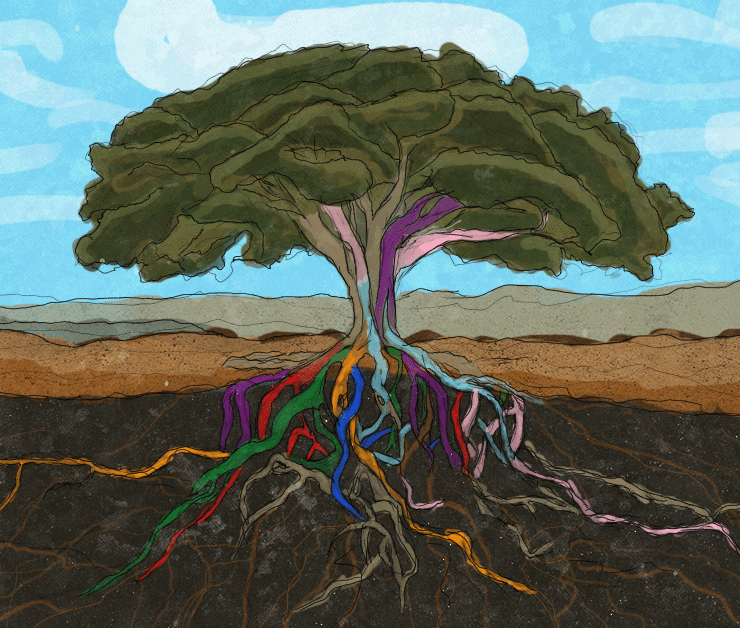
Image description: A human figure in a red and yellow room surrounded with glowing chat bubbles containing the words “It’s okay to feel this way”, “It’s safe to share”, “Talk to me”, “You are not alone”, and “Breathe”.
It’s a Thursday morning and I decided to be vulnerable over the phone. For the first time, I tried teletherapy. Unlike the traditional way of doing therapy in my past, where I met with a therapist in person, I chose to go the anonymous way.
Mental Health Uganda (MHU) was the recommended option. Panic engulfed me as I dialled the toll-free number—0800212121. As the phone rang, I listened to a caller tune that relaxed me from the panic I was feeling. The phone rang for about 30 seconds before a gentleman answered it. The question in my mind was, how does this even work?
Upon picking up the call, the gentleman identified himself as David and asked that I introduce myself. He assured me that the call was confidential and that none of my information would be shared outside of our phone call. He went on to tell me that the session usually lasts 45 minutes to an hour at most.
For the first time in a long time, I told someone the things I’ve kept to myself. We explored my grief, relationships, and dealing with everyday demands. I did most of the talking while David quietly listened.
“Would you like to talk about the issues surrounding your father’s death and how that left you feeling?” David asked
Something about his voice reassured me that I could be open, and I found myself speaking of issues that had long been buried in my head.
I am a face reader, so I am always conscious of people’s facial reactions when I speak. With the counsellor on the phone, I wasn’t worried about judgment, and he often asked where he needed clarification, which reassured me that he was listening.
In the end, he gave me recommendations and some insights to reflect on in preparation for our next discussion the following week.
Teletherapy always seemed useless to me; after all, why pay to call a therapist if you can just call your best friend? Also, being an emotional person, I always preferred in-person therapy. The only difference is that, just like with my best friend, I would censor myself to avoid sharing information that would get me judged.
With teletherapy, that was the least of my fears; even my name was fake—it was like writing an anonymous Reddit story, and at the end of the day, I still received the same attention and care as I would with an in-person therapist.
Teletherapy & Mental Health Uganda
Teletherapy is a new treatment in Uganda that gained traction only during the COVID-19 period. A number of organisations, including Mental Health Uganda, offer this service.
The organisation has been offering mental health services for close to 27 years. Its main role is to provide psycho-social support to people living with mental disorders. In 2018, after a partnership with Mental Health Norway, they developed the concept of offering support using phones.
“We developed the idea in 2018, but we fully implemented it in 2021 during the COVID-19 lockdown when we realised that many people needed support but could not physically meet,” Geraldine Kauma, the communications officer for Mental Health Uganda, explains.
Nanteza Teopista is a 26-year-old woman living with HIV/AIDs. When she was diagnosed with the disease, the first thing she was enrolled on was counselling, but she still battled with suicidal ideas.
“To me, no matter the constant reassurances I was being told by my family and a few friends, my mind was locked on the idea that my life had ended that day. At least life as I knew it,” Teopista explains.
For two years, she has been in and out of therapy, a feat that has been sustained by her father, who pays her dues to her therapist to ensure that she gets all the help she needs.
Teopista meets her therapist once a month, and sometimes, when it’s overwhelming, she schedules an online appointment.
“I honestly prefer using online therapy when dealing with a new person. I feel it’s safer and anonymous, but with the therapist I have had for the last two years, I prefer we meet physically; I feel she’s able to read me better when she’s seeing me,” Teopista explains.
The state of mental health issues in Uganda
The World Health Organisation (WHO) defines mental health as a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community.
Mental disorders vary and present differently. They include depression and anxiety, bipolar, personality disorders, schizophrenia, and other behavioural disorders like autism.
“Unless diagnosed, many people end up living out their lives with mental health challenges, and the stigma surrounding mental disorders prevents many from seeking the much-needed help,” explains Dr Hafsa Lukwata, the Acting Commissioner for mental health and control of substance abuse at the Ministry of Health.
In Uganda, mental health issues extend far beyond statistics, impacting individuals, families, and communities in profound ways. The prevalence of mental health conditions surpasses the global average, with a significant portion of the population experiencing these challenges between the critical ages of 11 and 24.
87% of Uganda’s population lives in rural areas, and there are 28 inpatient psychiatric units throughout the country—and only one mental referral hospital. Over 60% of the units are near Kampala, the capital of Uganda. Thus, those living in rural areas have little access to mental healthcare.
According to reports by Ugandan mental health professionals, 35% of Ugandans have a mental illness, and 15% of Ugandans require treatment.
“The most common mental disorder you find in Uganda is depression and anxiety. These are treatable, but the challenge is most Ugandans don’t believe in seeking help,” Moses Mpanga, a clinical psychologist and founder of MIND Nest Uganda (MNU), explains.
Unfortunately, the existing stigma surrounding mental health exacerbates the situation, leaving those affected isolated, ashamed, and often reluctant to seek the help they need.
“Apart from severe symptoms that may present a patient as a danger to themselves or those around them, and in this case, we look at suicidal ideation and thoughts, schizophrenia, oftentimes patients require therapy or outpatient treatment methods,” Dr Lukwata elaborates.
Not a silver bullet
In-person therapy is the conventional method of mental health care, and this occurs face-to-face between a client and a licensed therapist at a treatment centre or private office.
The practice of tele-counseling is still in its infancy in Uganda. It allows individuals to receive therapy and counselling services from licensed professionals via video conferencing, phone calls, or online messaging.
“Teletherapy provides a convenient and accessible alternative to traditional in-person therapy, especially for those who may have barriers to accessing physical therapy, such as geographic distance, physical limitations, or scheduling conflicts,” explains Lorna Nakabuye, founder of Kampala Counselling Services.
According to Afsan Mirza, a private mental health counsellor, though the practice is new in the country, the people she has counselled over the phone prefer it to physical meetups because they get to do it without the fear of anyone finding out and stigmatising them for it.
Many counsellors also noted that women are more into physical therapy and prefer to have a close relationship with their therapist, while men prefer to remain anonymous and hence prefer tele-counselling.
“We have noted that our tele-counselling services are mostly used by men in comparison to women, and for us, that’s a good step towards tackling men’s mental health in Uganda,” Kauma notes.
While tele-counseling has a good chance of being another milestone to open up access to mental health treatment, the cost is still a challenge for many Ugandans who need the service.
“The cost of access to therapy is between 50,000 to 300,000, and this is a session of maximum an hour depending on where you receive the service. That is very expensive for anyone who has to see a professional twice a week or more,” Teopista explains.
This also excludes many people who are unable to afford therapy in general. Organisations that offer the service free of charge still have to incur the costs from the providers, making it costly to provide.
One organisation, who sought anonymity, noted that the cost of attending to one client over the phone was the same as treating four people in person.
While one mental health expert needed to work with a group of 10-12 people for an hour in the community, teletherapy limited the counsellor to one person per hour. For an organisation that provides these services for free, it had to find a more cost-efficient alternative.
Furthermore, only 63.8% of Ugandans have access to phones, with much of that population living in urban areas. This means that most Ugandans have no access to phone technology and thus may struggle to access such services.
“Embracing teletherapy, especially in low-income communities, is a bit of a challenge because of issues that range from access to phones, connectivity to access to [the] internet,” says Dr Lukwata. ”This is frustrating and challenging for a person in need of the services.”
While teletherapy is beneficial, it doesn’t appeal to many. Although some organisations offer it at no cost—and where there is a cost, only a few can afford it—many people still prefer in-person therapy sessions within their communities.
“I don’t think I would be comfortable telling a stranger about my problems. How am I sure they relate? I’d rather tell the nurse in my community, but other than that, the women in my SACCO (Savings and Credit Co-operatives) are good confidants,” says Maureen Nanyonjo, a resident of Kirombe Lusaka.
Nanyonjo’s ideology is not far from that of many women in rural and suburban communities.
According to a report by StrongMinds Uganda, while their teletherapy program was often deemed more convenient and confidential than in-person programs, there was a general hesitancy around picking up calls from unknown numbers, mainly due to scamming and having outstanding loans.
The World Health Organisation recommends talk therapy in communities where treatment for depression cannot be accessed. This community treatment requires lay counsellors to deliver the group interpersonal psychotherapy model (IPT-G). With community treatment, participants learn from each other’s experiences and how they solve more practical challenges.
Currently, this service is free in Uganda, but it’s only available to women supported by StrongMinds Uganda.
In Nanyonjo’s group, a community member who was once part of a therapy group brought the idea to them, and now she holds the nickname ‘musawo,’ which translates to ‘medical personnel’ in the local language.
“If I tell the counsellor that I don’t have school fees or I don’t have what to feed my children, how will they help? How sure am I that they can even relate to my problems?” Nanyonjo says. “Here, when we sit in the SACCO on Sundays, If I tell them [my problems], they will give me a loan or even pass a basket for me. Telling me things will be okay is not the solution; talking to a counsellor will not put food on my table.”
From my background, I can understand Nanyonjo’s sentiments. There are days when your mental state is triggered by the lack of food or funds for your child’s school fees. However, I do appreciate that therapy, whether on the phone or in person, helps you communicate emotions with a person without the foundation of in-built perspectives from being close to you.
If I told any of my relatives the things I told my therapist over the phone, there were high chances I would be judged and crucified for feeling the way I did; the comfort of knowing that he didn’t know me helped me open up even on things I long thought I had moved on from.
Edited/Reviewed by PK Cross and Uzoma Ihejirika